Optimizing Falling Drop Hemoglobin Method by Comparing Capillary Versus Venous Blood and Determining the Stability of the Copper Sulfate Solution
DOI:
https://doi.org/10.14740/jh1337Keywords:
Hemoglobin, Hematocrit, Test, Anemia, Underdeveloped, Resource-poor, DevelopingAbstract
Background: Anemia is a global health issue that affects over 1 billion people and contributes to maternal mortality and birth defects. Low-resource, tropical areas face a dual challenge: high prevalence of anemia and inability to access affordable testing methods. The falling drop hemoglobin method has been developed by our lab to quantify hemoglobin concentration and assess anemia by timing the descent of venous blood in a column of copper sulfate solution, without using electricity or batteries. This research aimed to optimize the falling drop hemoglobin method by evaluating the use of capillary blood to reduce within sample variance and assessing copper sulfate stability to determine shelf life in expected working conditions.
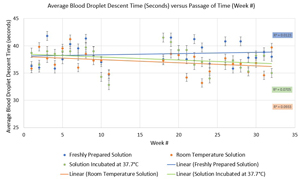
Methods: The falling drop hemoglobin method was performed on both venous and capillary blood samples collected directly from the fingertip by dispensing 44 µL of blood in a copper sulfate column. A microhematocrit was performed on the venous blood sample and converted mathematically to a hemoglobin level to serve as the standard. Copper sulfate stability was assessed for 32 weeks among three solutions: solution prepared fresh on day of testing, solution incubated at room temperature, and solution incubated at 37.7 °C.
Results: Capillary blood yielded higher average descent times and higher standard deviations than venous blood. Collecting precisely 44 µL of capillary blood proved challenging and impractical. In copper sulfate stability testing, freshly prepared solution yielded the highest average descent time. A one-way analysis of variance (ANOVA) test and Tukey’s honestly significant difference (HSD) post hoc testing revealed no significant difference between mean descent times of freshly prepared and 37.7 °C solutions (P = 0.26) and between room temperature and 37.7 °C solutions (P = 0.64), but a significant difference between freshly prepared and room temperature solutions (P = 0.04).
Conclusions: This study found that capillary blood did not present a more accurate alternative to venous blood in the falling drop hemoglobin test, and copper sulfate did not degrade over 32 weeks at 37.7 °C. This lends support for the current use of venous blood in the test, and for use of copper sulfate solution in tropical climates, where the test is most necessary, with a shelf life of at least 32 weeks.
Published
Issue
Section
License
Copyright (c) 2024 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.








