Evans Syndrome and COVID-19 Infection or Vaccination: A Systematic Review of Case Reports
DOI:
https://doi.org/10.14740/jh2058Keywords:
Evans syndrome, COVID-19, Vaccination, Hemolytic anemia, ThrombocytopeniaAbstract
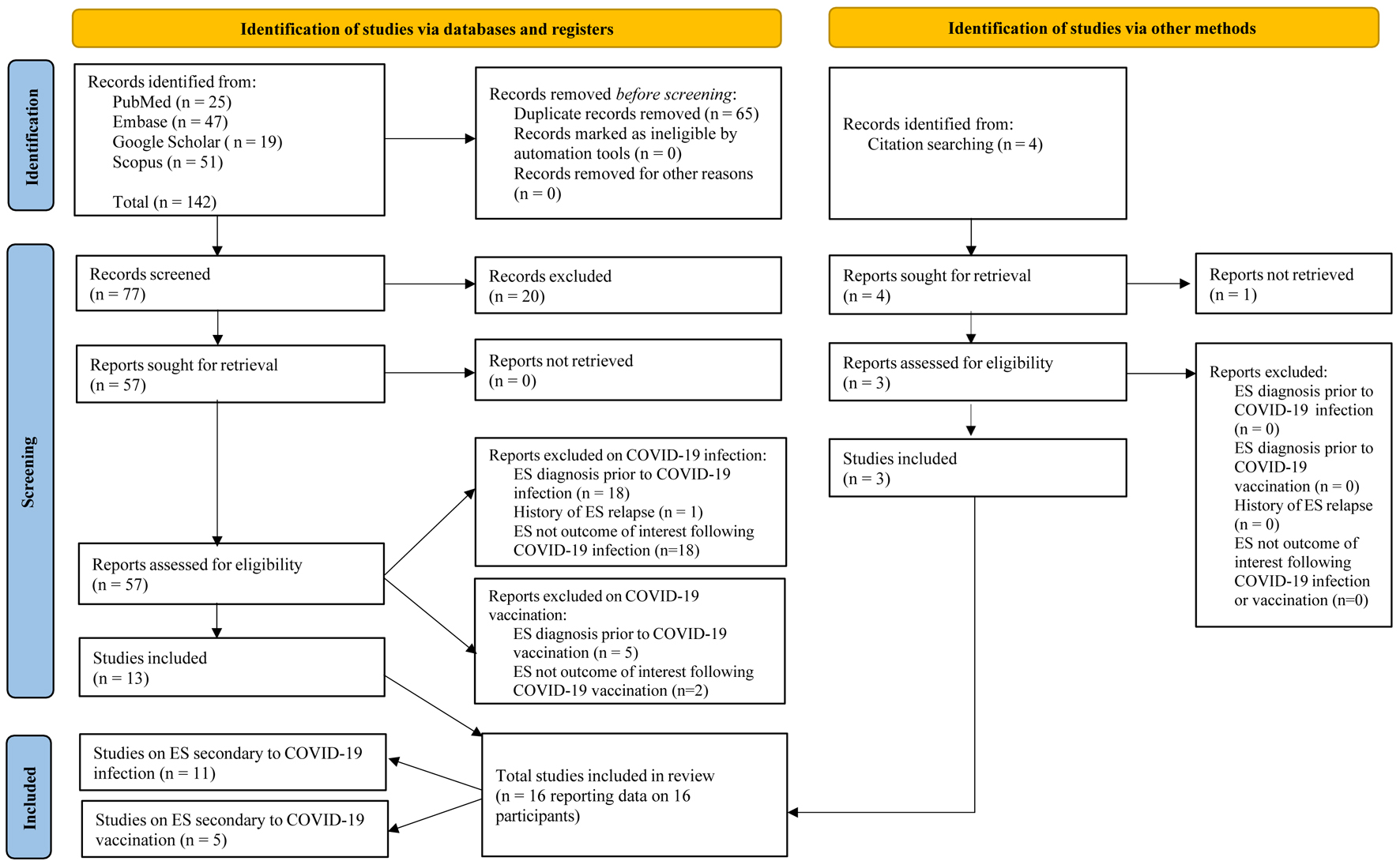
Evans syndrome (ES) is an autoimmune disorder of unknown etiology characterized by autoimmune hemolytic anemia (AIHA) and immune thrombocytopenia (ITP). In this systematic review, we analyzed the reported cases of ES secondary to coronavirus disease 2019 (COVID-19) infection or COVID-19 vaccination. We examined their clinical presentation, temporality between events, diagnostics tests, and treatment regimens. Our search in four databases from December 2019 to September 2023 yielded 16 case reports that met eligibility criteria for inclusion. COVID-19 and ES symptoms were defined to assess the timeline between infection/vaccination and ES onset. Finally, treatment efficacy was categorized as complete, partial, or no response based on standard hematological criteria. Eleven cases of ES were associated with COVID-19 infection, and five cases of ES were associated with COVID-19 vaccination. All 16 cases presented with anemia, thrombocytopenia, and a positive Coombs test. Four of the five patients from the vaccination subset were found to have an additional autoimmune disease as a comorbidity on presentation. For cases of ES secondary to COVID-19 infection, six patients had concomitant symptoms of COVID-19 and ES on presentation, and four patients had ES symptoms occurring from 5 days to 3 weeks following COVID-19 infection. The remaining case presented a patient with a 3-week history of ES symptoms before a positive COVID-19 test and further ES workup on admission. For the five cases of ES post-COVID-19 vaccination, all five patients presented with ES with a mean presentation time of 9 days following vaccination. Regarding treatment, intravenous immunoglobulin (IVIG) emerged as the primary regimen, administered in 13 out of the 16 cases. Among the infection-related cases, the most frequent treatment outcome was a partial response in both AIHA and ITP, observed in five of the 11 patients. In the vaccination-related cases, a partial response for AIHA and a complete response for ITP were noted in three of the five patients. Overall, while the evidence points to a temporal association especially between COVID-19 vaccination and the onset of ES, larger studies are necessary to strengthen these findings. In terms of management, early initiation of corticosteroids and IVIG appears effective as first-line therapies; however, standardized treatment protocols are needed to help reduce complications associated with COVID-19-related ES.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.








